Radiofrequency Ablation
Radiofrequency ablation is an unobtrusive system that destroys the nerve filaments conveying pain signals to the cerebrum. In Austin radiofrequency ablation gives enduring alleviation to individuals with interminable agony, particularly lower back pain, neck and ligament joints. If you endure intermittent pain and you’ve encountered great alleviation with a nerve square infusion, you might be a contender for radiofrequency ablation.
What’s radiofrequency ablation?
Radiofrequency ablation, likewise called rhizotomy, is a nonsurgical, non-intrusive technique that utilizes warmth to diminish or stop the transmission of pain. Radiofrequency waves remove, or “consume,” the nerve that is causing the agony, basically taking out the transmission of pain signals to the mind.
This strategy is normally used to treat ceaseless lower back pain and conditions, for example, joint inflammation of the spine also known as spondylosis and sacroiliitis. It is additionally used to treat neck, back, knee, pelvis and fringe nerve pain. The advantages of radiofrequency ablation include staying away from a surgical procedure, prompt relief from discomfort, practically zero recuperation time, a diminished requirement for pain relief medicine, improved work capacity, and a faster recovery time.
Who plays out the treatment technique?
The types of doctors who perform radiofrequency ablation are physiatrists (PM&R), radiologists, anesthesiologists, nervous system specialists, and specialists.
What occurs before treatment?
The specialist who will perform the ablation for lower back pain will survey your therapeutic history and past imaging to concentrate on designing the best area for the ablation. Be ready to ask any questions you may have during this consultation. Patients who take headache medication or a blood diminishing drug may need to quit taking it a few days before the procedure. Talk about any prescriptions with your primary care physicians, including the person who recommended the drug and the specialist who will do the infusion. The treatment is typically performed in an outpatient suite. Make plans ahead to have somebody drive you to and from the facility the day of the ablation.
Stage 1: Set up the patient
The patient lies on an x-beam table. A local sedative is utilized to numb the ablation treatment area. The patient encounters a little amount of discomfort all through the body. The patient stays conscious and mindful during the technique to give criticism to the doctor. A calming agent like Valium or Versed, is generally the main prescription given for this method.
Stage 2: Embed the needle
The method for nerve ablation is like that utilized for demonstrative squares. With the guide of a fluoroscope which is an extraordinary x-beam, the specialist coordinates a flimsy empty needle into the correct area. Fluoroscopy permits the specialist to watch the needle continuously on the fluoroscope screen to ensure that the needle goes to the ideal area. Differentiation might be infused to affirm the right needle area. Some distress happens, yet patients normally feel more weight than lower back pain.
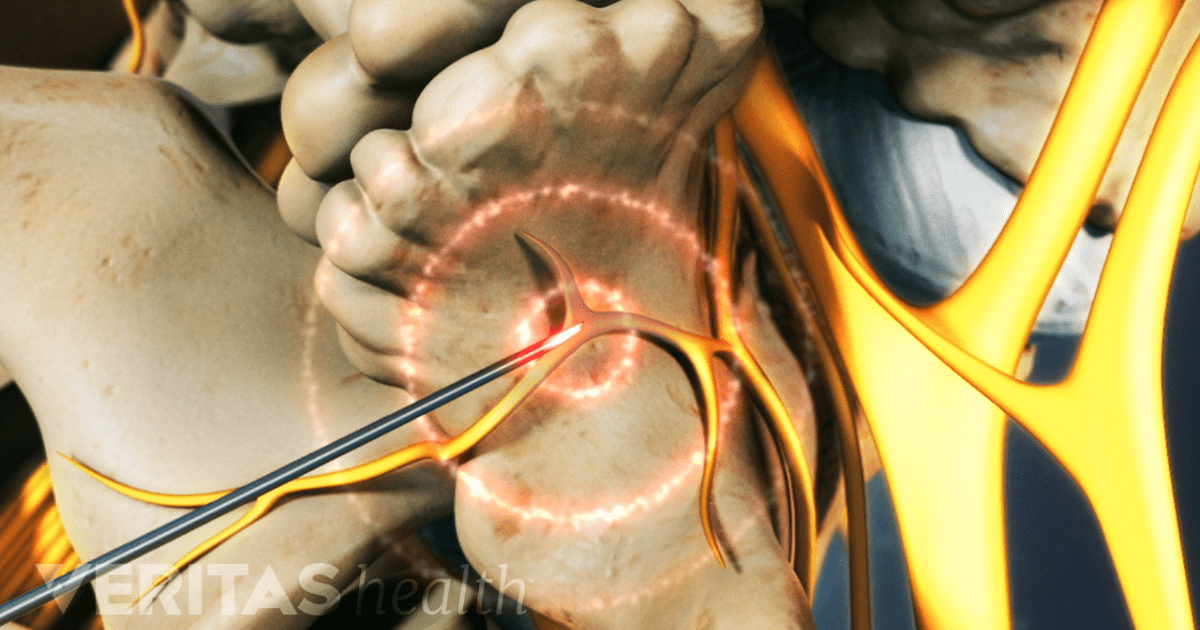
Stage 3: Convey radiofrequency current
When the needle is set up, the patient gets a desensitizing medicine. At that point, a radiofrequency current is pumped through the empty needle to make a little and exact consume, called a sore, about the size of a cotton swab tip. The current decimates the bit of the nerve that transmits lower back pain and upsets the nerve creating signal. The consume takes around 90 seconds for each site, and various nerves can be treated simultaneously.